
New market research reveals a deep divide between health plan executives recognizing the need to have full contextual awareness of a member’s health journey, which is critical to being able to personalize services that drive member engagement and quickly make the right care decisions to yield optimal outcomes for members, and tangible progress toward health plan objectives. Why? Payers are not strategically leveraging enough of their data.
“We’re at the point now — and we saw this in the market research — where healthcare organizations have a lot of data, but they don’t know how to integrate it into workflows to gain insights from it to build trust and personalization,” says Katherine Schneider, MD, CEO, Two Canoes Health.
Schneider participated in our webinar, The Year Ahead in Care Management, Utilization Management, and Population Health, on Jan. 18, 2024. The presentation also featured Julie Barnes, JD, CEO & Founder, Maverick Health Policy, and Ken Young, President & CEO, Medecision, and was moderated by Sage Growth Partners CEO Dan D’Orazio.
During the webinar, the executives shared an exclusive look at the new research results and discussed the following:
- The positive impact of personalization across care and utilization management functions
- The potential for contextual awareness in preparation for the new ePrior Authorization rule
- Personalization’s relation to health equity
- Workforce advantages of having the right contextual awareness to drive personalization
- The role contextual awareness has in fostering personalization and its impact on care management, utilization management, and population health
- Taking the first step toward contextual awareness and personalization


The Positive Impact of Contextual Awareness and Personalization
Medecision commissioned Sage Growth Partners to independently survey 53 health plan executives. The research shows that 95% of survey respondents say it is important to incorporate personalization into care management, but only 34% rate their health plan as very personalized.
“Now is the time for healthcare organizations to really drive personalization to achieve better outcomes and increase engagement with patients and members,” Young says.
Young and Schneider highlighted two extreme examples of lacking personalization in healthcare. One is the all too common scenario in which a woman goes through pregnancy and then, after giving birth, is invited to participate in a care management program simply because she had experienced a hospital stay. “That is just a complete lack of understanding where that person is in their health journey,” Young adds. An even worse misstep is outreach to someone after death.
In a counter-example, Young explains that personalized messages to help a member experiencing a behavioral health event schedule a follow-up appointment at the point of discharge, can have impactful results.
“Knowing what a person is experiencing and then guiding them to the next right care at that right time is about using the data available and personalizing the message to that individual,” Young says. “That outreach is equated to engagement rates north of 60% in that difficult population where the engagement rates are typically south of 10%.”
The Potential for Contextual Awareness and the New ePrior Authorization Rule
Barnes reviewed the new electronic prior authorization rule that the U.S. Department of Health and Human Services Centers for Medicare & Medicaid Services issued shortly before the webinar. She said that it will help healthcare providers serve their patients by more efficiently identifying which items and services are covered by insurance, and avoiding unnecessary utilization and expenses.
“It is really going to be a new day in America for how health plans and providers determine what should be covered by a health insurance benefit package,” Barnes says. “Health plans need to build out an API that allows electronic exchange of information so that providers know what health plans need to approve something for coverage – and there is a very automated dynamic between the exchange of what is requested and what is required to cover that request.”
When it takes effect on January 1, 2027, electronic prior authorization will be an important piece of the overall transformation health plans need to strive for. Having contextual awareness in the prior authorization puzzle will help make personalized, bespoke utilization management decisions for each member rather than relying wholly on predetermined guidelines.
Contextual Awareness and Personalization’s Relation to Health Equity
The speakers agreed that the industry trend of advancing health equity by working to connect all people with the resources they need to achieve the best possible health is important.
“Health equity is the ultimate form of personalization,” Schneider says. “Health equity is not merely a buzzword, but a regulatory focus and a key driver or North Star for health plans.”
Likewise, health plans can leverage that contextual awareness of a member’s health journey and overall situation to enable personalization capabilities that advance health equity. Both allow outreach to more effectively engage members at their individual health inflection point—rather than simply delivering the same messaging to everyone, regardless of their needs, Young adds.
“What’s important in putting it into action is to make sure that health plans are seeing the ROI when they invest in addressing social drivers of health,” Barnes says. That ROI comes from the ability to harness SDoH data within the care and utilization workflows in a timely fashion.
Workforce Advantages of Personalization
While much of the focus of contextual awareness and personalization in healthcare is aimed toward patients and members, the tools can also improve the overall experience for clinicians and caretakers. The chart below, in fact, illustrates that 99% of participating health plan leaders say incorporating personalization will have a high or moderate impact on reducing technical burdens on CM and UM staff, and 85% say it will reduce technical burdens on IT staff.
Also, 93% of health plan leaders say that incorporating contextual awareness and personalization into utilization management workflows will have a high or moderate impact on reducing provider abrasion.
“With the labor shortages we’re experiencing as clinicians, among both physicians and nurses, automation for reducing the administrative burden and the burnout that’s occurring to drive operational efficiencies and personalize the experience on the provider side will eliminate some of that abrasion,” Schneider says.
Contextual Awareness and Personalization’s Impact on Care Management, Utilization Management, and Population Health
Our research also found that health plan leaders believe incorporating personalization into care management, utilization management, and population health management workflows will positively impact those programs. Consider the following highlights:
- 98% of health plan leaders say personalization will have a high or moderate impact on improving member trust, 96% on reducing unnecessary utilization, and 96% on reducing costs
- 98% of health plan leaders say personalization will have a high or moderate impact on improving care manager efficiencies, 96% on reaching more members, and 97% on their ability to create custom care plans and journeys
- 98% of health plan leaders say personalization will have a high or moderate impact on improving member participation in population health, 98% say the same about increasing health literacy, and 96% believe personalization will improve outcomes
“When we talk to executives, we hear them say, ‘personalization is so important and can be impactful across the range of care management, utilization management, and population health,’” D’Orazio says.


Taking the First Step Toward Personalization
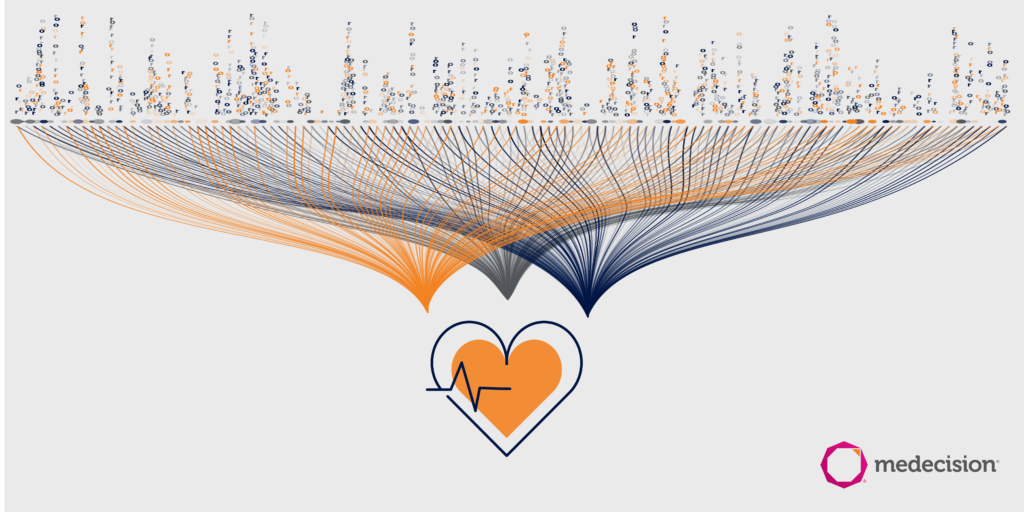
Personalization is driven by the ability to have a 360 degree view of the member’s health journey. This contextual awareness requires the intersection of data, analytics, workflow, AI, and patient or member engagement. That starts with the ability to ingest all data sets regardless of their file format – with automation and an orchestration engine – so health plans can focus on outcomes, not technology.
“The actionable first step is consolidating and understanding where all your data is and then prioritizing the data that will move the member to the next step. Not all data is created equal, so you have to prioritize it. But if you look at your point solutions data, your ADTs, labs, pharmacy, and claims data, you can create a holistic view of members and where they are in their journey,” Young says. “You’ll have much more real-time visibility into your members.”
The Year Ahead in Care Management, Utilization Management, and Population Health was the inaugural webinar in Medecision’s new monthly series. Our next webinar, The State of Utilization Management 2024, will take place on Feb. 15, 2024, at 11:30 ET. Register here.


About The Author: Medecision
Medecision is a leader in cloud-based, data-powered healthcare solutions, enabling risk-bearing entities to achieve improved health outcomes, optimized medical costs, reduced administrative costs, and personalized engagement. Our Aerial platform supports over 10% of the U.S. population, marking a significant milestone in advancing healthcare efficiency and effectiveness.
More posts by Medecision