
Legacy care management (CM) technologies and workflows are creating challenges for healthcare organizations looking to expand their programs—which negatively impacts clinical outcomes, financials, and overall CM results. That reality has some leading executives examining new approaches.
“We’re rethinking how we provide care management,” says Robert Groves, MD, Executive Vice President & Chief Medical Officer, Banner|Aetna. “Historically, care management has been based on outreach phone calls, and there are many folks who we simply can’t reach by that method. We’re shoring up care management through data and digital strategies to improve our ability to contact people, onboard them, and encourage them to sign up for services that are useful to them.”
Groves participated in the Becker’s Hospital Review webinar, The Top Care Management Barriers — And How to Tackle Them, on March 19, 2024, with Jessica Chaudhary, MD, Medical Director, Elevance Health, and Kenneth Young, President & CEO, Medecision.
| What New Research Reveals about Care Management
Read the Report
|
Elevance is also increasingly leveraging digital tools to move toward personalization. “Our goal is to engage lower-risk individuals and reach them earlier, before health events become a crisis,” Chaudhary says.
Achieving that personalization requires establishing contextual awareness with a combination of the right tools and multiple data sets. “It’s not just telephonic outreach, it’s not just digital,” Young says. “It’s merging both to create contextual awareness that makes outreach personalized.”
During the webinar, the experts discussed:
- Top barriers to expanding CM programs
- The urgent opportunity: overcoming top barriers to engage more members
- Where healthcare organizations are already making an impact with CM
Top Barriers to Expanding Care Management Programs
New Medecision market research found that the single biggest barrier to activating more people in CM programs is the lack of tools to engage them in their own healthcare.
“The perpetual challenge has been how to get people engaged,” Chaudhary says. “Once they are engaged, they really tend to stick with the program, and they appreciate what we have to offer. But that first step is getting their foot in the door.”
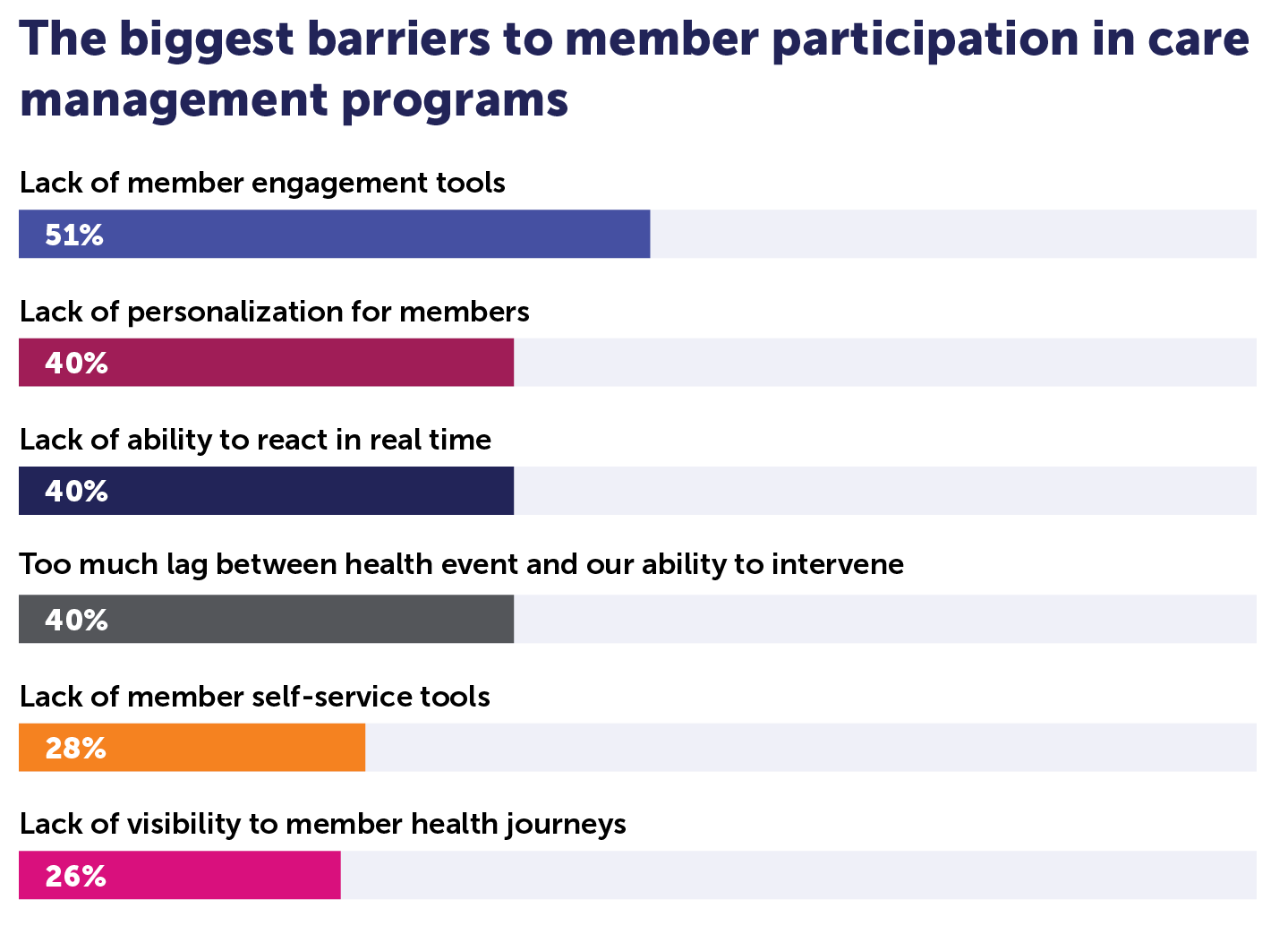
Healthcare leaders also rank the lack of personalization, the lack of an ability to respond in real-time, and the lag between health events and their ability to intervene, as barriers to engaging more members in care management programs.
In addition to what our research found, Elevance has thus far learned that success in increasing participation in CM programs rests on communicating effectively with patients or members. “One of the barriers is communication — communication between providers, between caregivers, between individuals and their families,” Chaudhary explains. “So one way to leverage care management is to intervene at their times of need.”
The Urgent Opportunity: Overcoming Top Barriers to Engage More Members
As healthcare organizations increasingly reconsider their CM programs, more are working to leverage data across all appropriate sources. Those include ADTs, lab results, call center activity, claims, remote monitoring, social determinants of health, and fitness tracking information.
Strategically leveraging those data sets is critical to understanding how and when to conduct outreach to low- and rising-risk members. Putting the data to work also creates an enormous opportunity to reduce unnecessary utilization and associated medical and administrative spending.
Given the challenges in leveraging these data sets, it’s not at all surprising that more than one-third of the leaders participating in our survey say their organization accommodates fewer than 40% of expensive, high-risk members in their CM programs. Half say they engage fewer than 40% of rising-risk members.
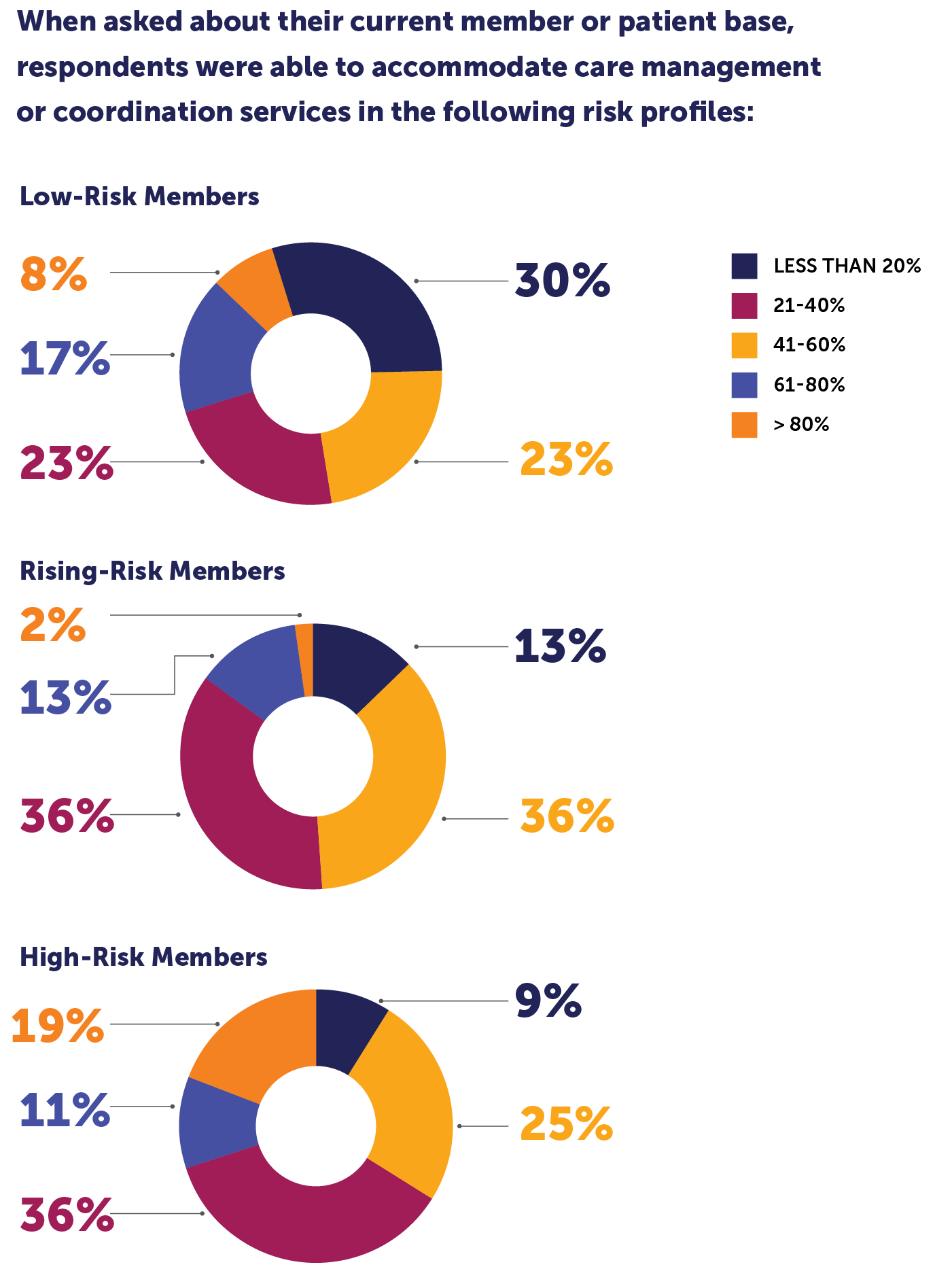
“Healthcare organizations need ways to manage the entire risk paradigm, from high-risk to rising-risk to low-risk,” Young says.
Health systems and health plans also have to ensure that when a patient or a member in any risk category requires an outreach or intervention because their risk profile has changed, care teams can access the necessary information to respond in a timely and personalized manner.
“Data is critical. Otherwise, we’re flying blind, which we’ve done for years, but we shouldn’t be afraid to leverage tools that help people take steps that are ultimately in their best interest,” Groves says. “We know the right strategies can improve the rates of engagement. We know that the inflection point is an important opportunity to do that.”
Further, health plan and health system executives rethinking CM strategies should understand the criticality of strategically leveraging a wider range of data types and cutting-edge technologies to reduce administrative and medical expenses, drive personalization, and improve health outcomes for members and patients.
“If you don’t leverage all of the data available to know the best way to conduct outreach to people and understand where they are in their journey, you lose credibility,” Young says. “And once you lose credibility, it’s very difficult to regain.”
Where Healthcare Organizations Are Already Making an Impact with CM
Groves and Chaudhary shared successful CM initiatives during the webinar, with a particular focus on metabolic disease and suicide prevention, respectively.
Banner|Aetna is working to address “the other pandemic” of metabolic disease in this country: obesity, hypertension, truncal obesity, elevated triglycerides, pre-diabetes, and diabetes mellitus. The initiative began by developing a coherent plan to ensure patients and members can easily find services and understand how to access care. “That’s an important element of our strategy going forward,” Groves says. “We will continue to identify new ways to address the access problem from a care management perspective.”
Groves adds that Banner|Aetna made the unique commitment to transition its CM functions to the provider side of its integrated delivery network. “We’re having great success because the outreach is now coming from the delivery side,” Groves says. “We cooperate and coordinate efforts.”
While it’s still a nascent program, Banner|Aetna also created a cooking show experience to address metabolic syndrome alongside loneliness and isolation simultaneously. The organization invites patients or members at high risk for these health problems to a series of cooking classes hosted by both a chef and a dietician who teach them about food preparation and nutrition, then give them those ingredients to take home and cook for themselves and their families.
“Frankly, even I underestimated the reaction to this program,” Groves says. “They tell their friends, they tell their families, they talk about it, and because it’s experiential learning, they don’t forget it.”
Banner|Aetna intends to begin formally measuring the impact this year. However, Groves says self-reported data already shows that patients are losing 5% to 10% of their body weight and are lowering A1C scores by a point or more.
Elevance Health, for its part, established a suicide prevention program in 2018 to serve adolescents and young adults. “We had to do something about the staggering rates of suicide,” Chaudhary says. “But monitoring the trend is not enough. This program is really based on predictive analytics that include hundreds of different variables.”
Those factors include people who have been at different levels of care, with different diagnoses, such as substance use, and medical issues not limited to psychiatric care. Elevance determined that medical issues linked to higher rates of suicide include chronic pain, pain syndromes, headaches, and even conditions such as asthma, which Chaudhary says lean toward social drivers of health as well.
By leveraging its data and analytics, Elevance identified people at the highest risk of either attempting to hurt themselves for the first time or those likely to try again. Then, the organization started conducting personalized and proactive outreach to the at-risk individuals and found that it had a five-month timeframe in which to make a notable impact.
Elevance has since expanded the program to include people ranging in age from 10 to 100 years old. “We’ve achieved a reduction in suicide attempts and events by more than 15%,” Chaudhary says. “We’ve seen thousands of people actually take a different trajectory.”
Read the article reporting on the previous webinar in our monthly series, Utilization Management is Fragmented and Frustrating: Here’s How New CMS Rules Can Help, on the Medecision blog.



About The Author: Medecision
Medecision is a leader in cloud-based, data-powered healthcare solutions, enabling risk-bearing entities to achieve improved health outcomes, optimized medical costs, reduced administrative costs, and personalized engagement. Our Aerial platform supports over 10% of the U.S. population, marking a significant milestone in advancing healthcare efficiency and effectiveness.
More posts by Medecision