
Legacy utilization management (UM) technologies and workflows create a number of challenges. Even though health plans have enormous amounts of information, UM tools are not very effective at fully integrating key data sets into existing workflows. As a result, health plans are struggling to manage utilization, drive down medical costs, and improve outcomes for members.
“There have been strides in integrating various types of data into utilization management workflows, but there’s a lot of room for improvement,” says Kenneth Young, President and CEO, Medecision.
Young participated in our webinar, The State of Utilization Management, on Feb. 15, 2024, with Julie Barnes, JD, CEO & Founder, Maverick Health Policy. During the discussion, moderated by Stephanie Kovalick, Chief Strategy Officer of Sage Growth Partners, the speakers shared relevant UM results from our new survey of 53 health plan leaders, The State of Utilization Management, Care Management, and Population Health 2024.
“The research shows that legacy utilization management tools are ineffective at providing the real-time data necessary to be successful, and they create a number of UM pain points,” Kovalick says. “Not only that, but the policy and regulatory landscape continues to evolve, and plans may or may not have the resources to live up to new expectations.”
Key UM-Related Takeaways from the Discussion
During the webinar, the experts shared insights and perspectives on the following factors shaping UM requirements and technology needs for health plans:
- Regulations are evolving: UM, prior authorization, and interoperability
- The need to transform utilization management quickly is clear
- AI and automation have great potential to optimize and accelerate UM
Regulations are Evolving: UM, Prior Authorization, and Interoperability
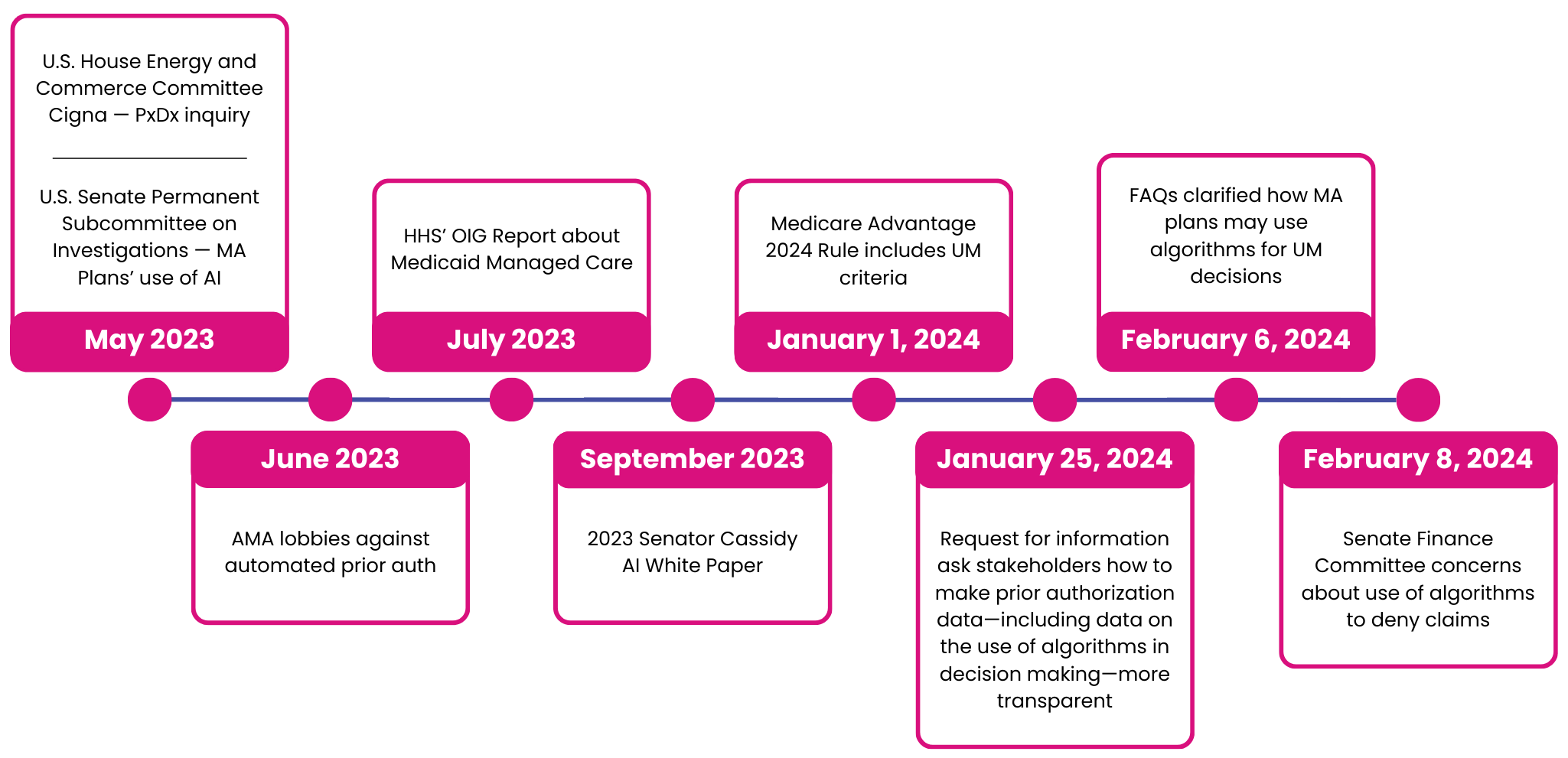
The speakers walked through the timeline of regulatory changes relative to utilization management, prior authorization, and interoperability.
| AI, Algorithms, and Prior Authorization
|
For UM, the Centers for Medicare and Medicaid Services’ 2024 Medicare Advantage and Part D Final Rule includes UM requirements. Medicare Advantage (MA) plans, for example, are mandated to “establish a Utilization Management Committee to review policies annually and ensure consistency with traditional Medicare’s national and local coverage decisions and guidelines.”
When it comes to prior authorization, Barnes notes that the federal government has been investigating technology-supported processes for about a year. The Health and Human Services Department’s Office of Inspector General (OIG) issued a scathing report in July 2023. In that document, OIG showed how some Medicaid Managed Care Organization plans were using prior authorization processes to improperly deny high rates of medically necessary services from being covered.
CMS issued its Interoperability and Prior Authorization Final Rule to “reduce overall payer and provider burden and improve patient access to health information while continuing CMS’s drive toward interoperability in the healthcare market.” That rule requires health plans to implement the Patient Access API and the Provider Access API to enable a more seamless exchange of health data.
“The regulations that exist were written to promote data sharing,” Young says. “That’s why we chose to be API-first. Health plans need the ability to interact with data across ecosystems. There isn’t a one-size-fits-all approach.”
Ultimately, the new rules mean health plans have to step up their focus on UM to overcome barriers associated with ineffective legacy tools (see chart below). “Health plans now have to make coverage decisions faster, provide reasons for denials, and track all of it,” Barnes says.
The Need to Transform UM Quickly is Clear
Health plans need to upgrade from legacy systems to modern UM technologies to keep pace with the evolving regulatory landscape. Medecision research found that 98% of survey respondents say it’s important that workflows and processes are able to comply with existing and future regulatory requirements, but 88% of health plan leaders say poor integration of data into workflows is a barrier to regulatory compliance.
Compliance with federal regulations is also essential to overcoming the common UM obstacles our research uncovered. Health plans must address those barriers because they are currently causing a number of frustrations, as seen in the chart below.
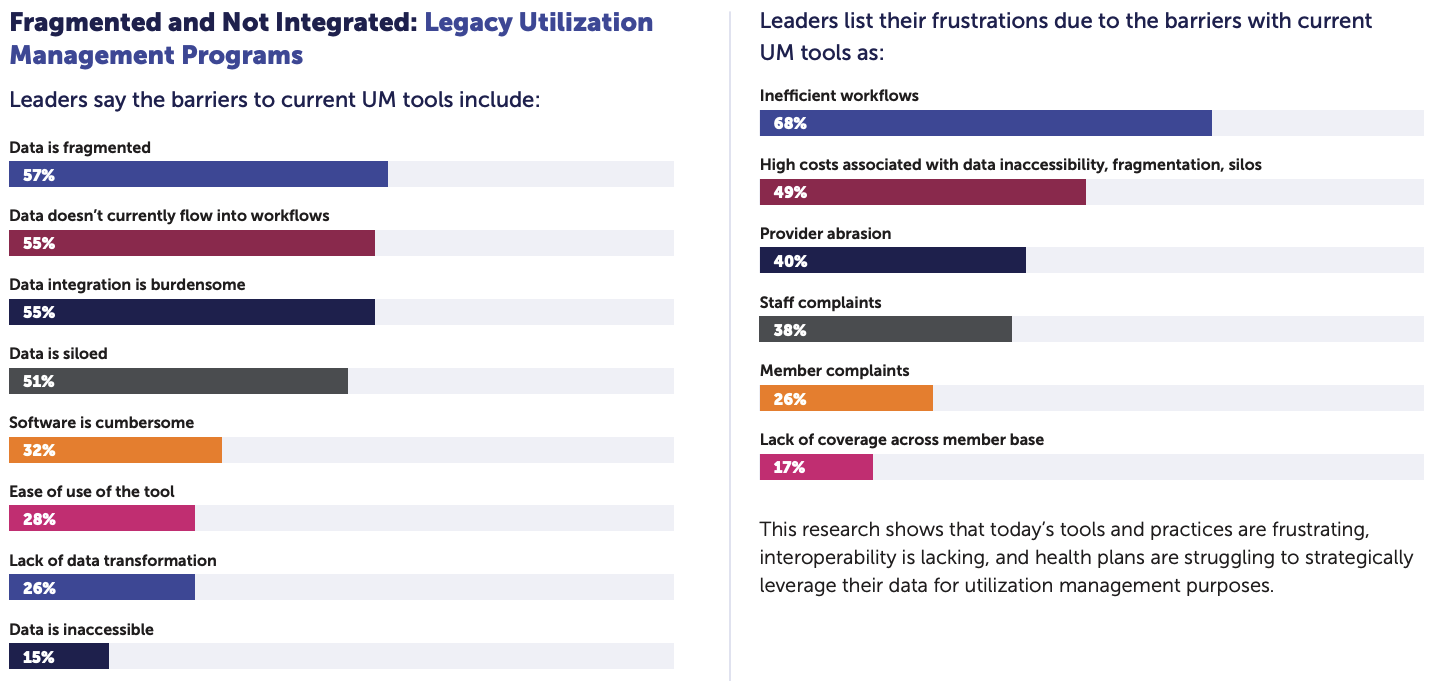
Our survey results show that older UM tools and strategies are also leaving data fragmented rather than integrated and useful. Our research also finds that UM software is overwhelmingly cumbersome and leads to inefficient workflows, high costs associated with difficulties accessing data, and provider abrasion.
“There’s a real and urgent need to transform legacy utilization management tools and workflows to provide quicker decisions about the individual member so health plans can ensure the right care at the right time,” Kovalick says. “The only way health plans can do that is to leverage a wider range of data sets—from medical to social determinants, behavioral, genetic, and others—to really drive efficiencies and reduce costs.”
AI and Automation Have Great Potential to Optimize and Accelerate UM
AI and automation hold considerable promise to drive greater efficiencies than legacy utilization management tools have done. More than half of health plan leaders participating in our survey are optimistic that AI and machine learning advancements will be important moving forward. Specifically, the research highlights that survey respondents believe AI will enable health plans to:
- Optimize UM
- Accelerate UM decisions
- Reduce unnecessary medical care
- Drive down costs
- Ease administrative burden on their workforce
To leverage those benefits, the speakers noted that health plans need to find ways to harness AI for manual processes. “Health plans cannot afford just to increase healthcare costs,” Young says. “Payers have to drive efficiencies when implementing new technologies and determine how to leverage relevant data in real-time.”
As health plans embrace advancements in AI and automation, it’s also important to understand that data is the most critical piece. AI and automation are only as good as the breadth and depth of the data sets those systems can access.
“Implementing a data platform is critical to ensuring that health plans can properly orchestrate UM processes with the proper AI governance,” Young says. “Making that investment is the first step. If you get the data right you can leverage it in real-time to make correct decisions quickly and have visibility across all of your partners.”
Read the article reporting on the previous webinar in our series, Why Health Plans Need to Close the Personalization Gap – Now, on the Medecision blog.



About The Author: Medecision
Medecision is a leader in cloud-based, data-powered healthcare solutions, enabling risk-bearing entities to achieve improved health outcomes, optimized medical costs, reduced administrative costs, and personalized engagement. Our Aerial platform supports over 10% of the U.S. population, marking a significant milestone in advancing healthcare efficiency and effectiveness.
More posts by Medecision